Allied & Other
Allied & Other Health Professionals Play Key Support Roles for Individuals with FASD
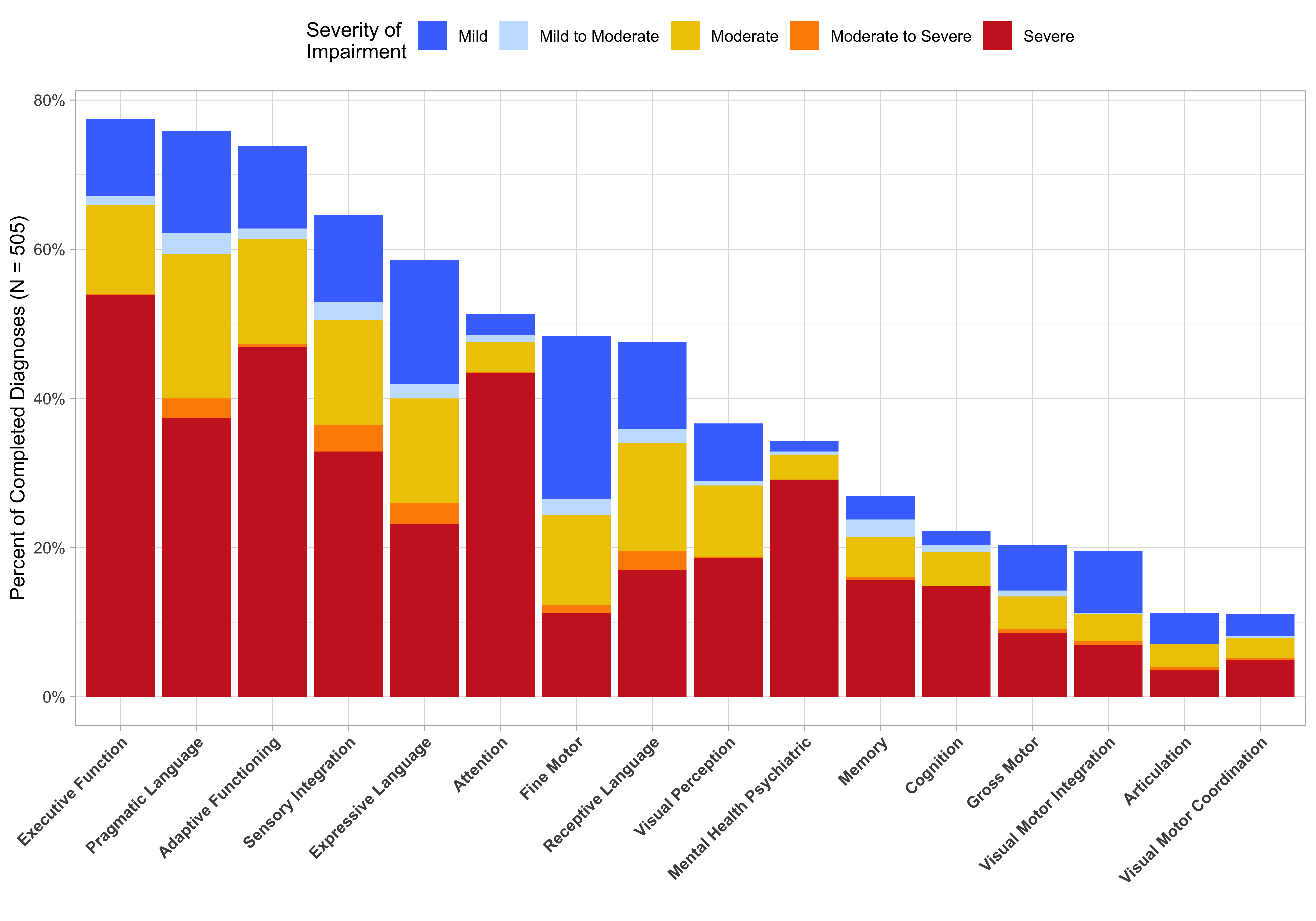
FASDx Services LLC data used with permission.
A comprehensive FASD diagnostic team process is one the State of Alaska currently endorses. However, a primary care or specialty medical professional could send referrals to allied health colleagues and use their combined report findings, in addition to a physical exam, to formulate a diagnosis as well.
For adults, we recommend beginning with a neuropsychology evaluation. However, since social language challenges are so common, it would be ideal if an adult could also be assessed by a speech language pathologist since difficulties in this area often makes the individual very vulnerable to the influence of others and can contribute to their difficulties with independent living.
The following key considerations are based on ‘lessons learned’ by the Anchorage FASD Diagnostic Team and do not represent all possible issues or concerns for each allied health professional group. We do endorse the idea of more health professionals in Alaska becoming ‘FASD-informed’ in their respective practice areas!
Key Considerations for Occupational Therapists
Occupational therapists (OTs) are a health profession that we consider to be the ‘unsung heroes’ among health professions. Their name can be confusing to the public and their expertise in brain function is often under-appreciated. For children who are having behavioral difficulties, especially those under age 5, an occupational therapy treatment strategy can often be an excellent alternative to medications or traditional behavioral health therapy. Occupational therapists use assessment tools, observation, and interviews to evaluate various areas of brain and life functioning including: sensory processing, fine motor, oral motor, visual motor, visual perception, and self-help skills (as compared to same age peers.) Their goal is to assess abilities and the environment, make recommendations, and provide interventions to improve the patients' everyday lives in the context of home, leisure activities, and school or work.
Sensory processing difficulties can manifest as hyperactivity, distractibility/attention issues, food texture/taste issues, and deep pressure-seeking behaviors to name a few areas. The sensory system can be ‘wired’ in a way that someone has over or under sensitivity OR sensory-seeking behaviors. There can be an overlap in this symptom area with individuals who experience autism. However, a full scope OT evaluation may reveal areas of impact that are not found in individuals with autism but are common in those with PAE. Key considerations for OTs related to FASD:
- Ensure that a full scope OT assessment is done for anyone who may have PAE as impacts may not always be obvious.
- Use testing tools pages 18-22 that are known to best discern areas of function that may be impacted. For example, the Peabody Developmental Motor Scale assesses IF a child can do a certain skill but may not assess HOW WELL…this matters for someone with PAE.
- Recognize that a trauma history can impact sensory responses and motor, emotional regulation, or self-help skill delays.
- Seek FASD-related continuing education opportunities so that standardized test results interpretation can be made through that lens (1 in 20 school age children are likely to have an FASD today).
- NOTE- American Occupational Therapy Association (AOTA) Critically Appraised Papers series: FOCUSED QUESTION Does a neurocognitive habilitation group therapy service improve executive functioning and emotional and social problem-solving skills in children with fetal alcohol syndrome (FAS) and alcohol-related neurodevelopmental disorder (ARND) compared to a no treatment group using the Behavior Rating Inventory of Executive Function (BRIEF) and the Roberts Apperception Test for Children (RATC)?
- Consider using an evidence-based program for children with an FASD such as:
- PACT a group program designed to improve behavior regulation skills, executive functioning, and parent effectiveness.
Key Considerations for Speech Language Pathologists
Speech Language Pathologists (SLPs) are another allied health group that contributes significantly to the assessment and services for individuals with PAE. The amount of human brain that is dedicated for the ‘communication center’ is vast compared to other functional areas so it is very common for individuals to have difficulty in one or more of the areas of communication. Many people consider articulation (difficulty with speaking certain sounds) to be the area most impacted and do not understand that language is most often the issue.
There are three primary areas of language that should be assessed: receptive, expressive, and social/pragmatic. Receptive language begins during the prenatal period as the baby can hear mom/dad and others while still in the womb. As one example, if the brain connections are not ‘wired’ correctly, it is possible that an individual may have difficulty understanding longer sentences and may react to only part of the intended message (i.e. the first or last part of the message). Expressive language is the ability to organize thoughts/words and put them into understandable sentences. An example of difficulty may be that someone has trouble responding quickly when spoken to, cannot tell a story with a beginning/middle/end, or shuts down using placeholders such as “I forget” or “I don’t know” when they feel pressed for a speedy response. Social/pragmatic language is demonstrated by an ability to correctly ‘read’ situations and body language or facial expressions, learn how to act in certain social situations, stay safe, problem solve, and maintain relationships. Social language difficulties can overlap with those who experience autism. One important difference can be that an individual who experiences an FASD usually has a high desire to be social and connect with people but does not ‘read’ situations correctly. This can become much more obvious as they get older. Key considerations for SLPs related to FASD:
- Ensure that a full scope SLP assessment is done for anyone who may have PAE as impacts may not always be obvious (do not neglect using age-appropriate social language assessment)
- Use testing tools pages 18-22 that are known to best discern areas of function that may be impacted (i.e. The OWLS is a tool that may not adequately assess potential areas of impact for individuals with an FASD)
- Recognize that a trauma/neglect history can impact all areas of communication
- Seek FASD-related continuing education opportunities so that standardized test results interpretation can be made through that lens (1 in 20 school age children are likely to have an FASD today)
- Consider implementing Good Buddies, an evidence-based program for social language learning/therapy for children ages 6-12 who experience an FASD.
Key Considerations for Physical Therapists
Individuals with prenatal alcohol exposure (PAE) often have motor and joint issues that can benefit from the services of physical therapists. The Anchorage FASD Diagnostic Team observed individuals who had joint laxity, flat feet, truncal orthopedic abnormalities (i.e. scoliosis or pectus deformities), and motor dyscoordination issues. Clinical manifestation of the PAE may begin in infancy with a baby having ‘low tone’ (i.e. the infant may avoid tummy time, not be able to lift their head, or sit without support by 8 months of age). An infant/child may also demonstrate early evidence of fine motor delays with reaching for or grasping objects. These difficulties can translate into self-care skill delays. As they age, children with flat feet may begin to complain of leg or hip pain (that is related to their feet) that may benefit from orthotics. Key considerations for PTs related to FASD:
- Ensure that a full scope PT assessment is done for anyone who may have PAE as impacts may not always be obvious
- Use testing tools pages 18-22 that are known to best discern areas of function that may be impacted. Of note, ongoing research is underway to determine best tools. A recent Canadian evaluation Accuracy of Motor Assessment in Fetal Alcohol Spectrum Disorders indicated that the BOT-2SF was an inaccurate assessment tool for FASD diagnosis. The MABC-2 (Motor Assessment Battery for Children-2) total motor score was the most accurate using current (Canadian) guidelines, though its sensitivity was still low. Further investigation into inclusion of single subtests and/or using a less conservative cut-off (in the Canadian Guideline) is warranted.
- Recognize that a trauma history may impact motor development
- Seek FASD-related continuing education opportunities so that standardized test results interpretation can be made through that lens (1 in 20 school age children are likely to have an FASD today)
Key Considerations for Social Workers
Social workers may have contact with individuals who experience an FASD through the Office of Children’s Services or Office of Public Advocacy systems, in healthcare practices/hospitals as medical or behavioral social work service providers, in behavioral healthcare settings as therapists, or in adult-related service systems such as criminal justice or disability/supported living systems. As a profession that is concerned with helping individuals, families, groups and communities to enhance their individual and collective well-being, social work aims to help people develop their skills and their ability to use their resources and those of the community to resolve problems. The National Association of Social Workers (NASW) Foundation has been involved in the Centers for Disease Control & Prevention (CDC) Collaborative for an Alcohol-Free Pregnancy and developed strategies to help support social workers’ vital role in helping to reduce risky drinking behaviors through universal alcohol use screening. They also developed FASD Clinical Resources for Social Work Practice. It is imperative that social work providers become FASD-informed providers as they WILL intersect with clients who experience this disability across all settings in which they serve.
- Ensure that a social work assessment includes questions related to potential prenatal alcohol exposure (for both adults and children)
- Learn to use open-ended questions that allow for more detailed answers and that may help to reduce the stigma associated with maternal prenatal alcohol use
- Note that many of the behaviors that are problematic for clients in systems (i.e. missed appointments, poor social interaction skills, poor organizational skills, poor memory, poor initiation or shifting of assigned tasks, and emotional regulation difficulties can all be manifestations of the brain-based disability seen in FASD)
- Recognize that a trauma/neglect history may contribute to the clinical presentation for someone with PAE and make it more difficult to determine underlying brain-based differences until after adequate trauma therapy has been completed
- Support policies that can remove barriers to obtaining accurate prenatal alcohol exposure information (i.e. many states have policies that discourage women with alcohol and other addictions from accessing the health care system due to substance/alcohol reporting concerns)
- Seek FASD-related continuing education opportunities as FASD is common (1 in 20 school age children are likely to have an FASD today) and may be multigenerational
Key Considerations for Dental Providers
Key Considerations for Dieticians
Dieticians can play a key role in helping families/caregivers and individuals who experience an FASD to navigate some of the difficulties they may encounter. Individuals who experience an FASD may have a variety of challenges that can impair their ability to regulate oral intake or weight. They may have oral sensory issues that interfere with the consumption of specific textures or flavors. They may have brain-based appetite regulation differences that make it difficult for them to know when they are either hungry or full. As a result, they may be under or overweight. For a good summary consider reviewing, Abnormal Eating Behaviors are Common in Children with Fetal Alcohol Spectrum Disorders.
It is not uncommon for infants with prenatal alcohol exposure (PAE) to have ‘failure to thrive’ commonly due to a motor difficulty (poor sucking) but potentially also due to the appetite regulation issue. As the child ages, they may experience fine motor or other coordination skills that makes it more difficult with self-help feeding or simple meal prep skills. In adulthood, they may also have great difficulty with the organizational (executive function) skills needed for financial management, meal planning, grocery shopping, planning and cooking meals, and safe food handling. Because individuals with an FASD must work much harder (from a brain perspective) to make it through their day, they may crave carbohydrates at a higher than typical rate as this is the brain calling for more fuel to sustain itself! Dietary counseling needs to take all of these potential FASD-related actors into consideration.
- Ensure that a dietary assessment includes questions related to potential prenatal alcohol exposure (for both adults and children)
- Learn to use open-ended questions that allow for more detailed answers and that may help to reduce the stigma associated with prenatal alcohol use
- Note that many of the behaviors that are problematic for clients in systems (i.e. missed appointments, poor social interaction skills, poor organizational skills, poor memory, poor initiation or shifting of assigned tasks, and poor follow through on instructions can all be manifestations of the brain-based disability seen in FASD)
- Seek FASD-related continuing education opportunities as FASD is common (1 in 20 school age children are likely to have an FASD today)
- One area of significant interest is that of choline supplementation research for postnatal neurodevelopment support. Go to: Four-year follow-up of a randomized controlled trial of choline for neurodevelopment in fetal alcohol spectrum disorder.
- In addition, ongoing international research is being conducted to assess the contribution of maternal nutritional status in relation to physical and neurobehavioral outcomes associated with prenatal alcohol exposure, and to test the benefit of maternal second and third trimester supplementation with multi-nutrients with or without choline with respect to risk for FASD in the offspring.
